Symptoms, diagnostic methods, causes and treatment of Diabetic Retinopathy at a glance
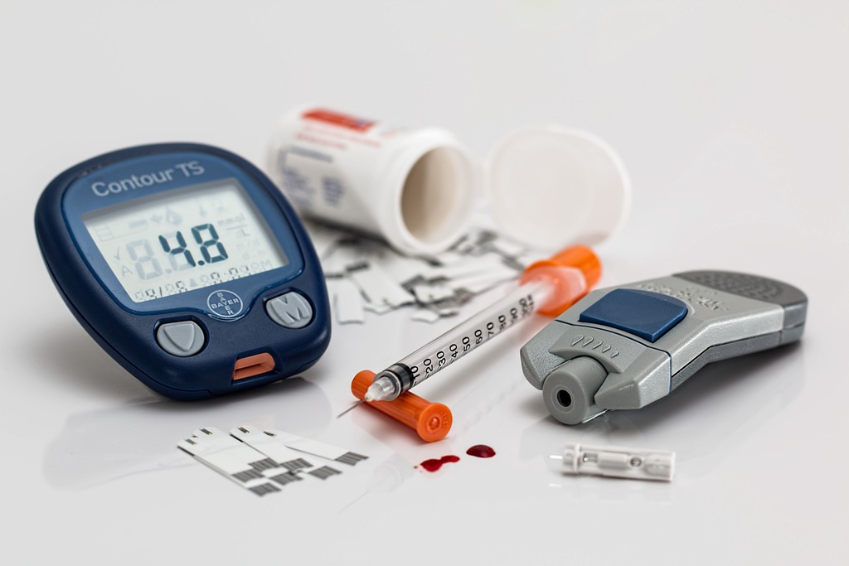
Diabetes mellitus one main cause and risk factor for Diabetic Retinopathy
Diabetic Retinopathy at a glance
Diabetic retinopathy is an eye disease that occurs as a result of diabetes mellitus. It affects the blood vessels of the retina and can lead to loss of vision.
High blood sugar levels damage the blood vessels, which can cause haemorrhaging, swelling and the formation of new, abnormal vessels in the retina, which can ultimately impair vision.
The main symptoms of Diabetic Retinopathy
The main symptoms of diabetic retinopathy include, for example:
- Visual deterioration: Including blurred vision and loss of focus
- Distorted or blurred vision: which can lead to altered perceptions
- Flickering or flashes in the field of vision: Possible signs of vascular changes
- Scotomas – dark or empty areas in the field of vision: which can indicate retinal damage
- Difficulties with colour perception: Significant impairment in recognising colours
- Difficulty reading: Due to impaired vision
- Changes in the peripheral visual field: Reduced lateral vision
- Pain or pressure in the eye: As a possible sign of complications
Sudden loss of vision can also occur. Obviously a very serious symptom that requires immediate medical attention.
The most important options and methods for diagnosing Diabetic Retinopathy
These diverse diagnostic options for diabetic retinopathy help doctors to recognise changes in the retina at an early stage and protect vision:
- Eye examination: looking directly at the retina to identify changes
- Fundus photography: Images of the retina for detailed analysis of microaneurysms, haemorrhages and swellings.
- Optical coherence tomography (OCT): Layer-by-layer imaging of the retina for precise measurement of swellings and changes.
- Fluorescein angiography: Contrast-based visualisation of blood vessels to detect leaks and abnormalities.
- Visual field test: Examination of the peripheral visual field for signs of retinal damage.Electroretinogram (ERG): Measurement of retinal cell activity to assess visual function.
- Total body examination: Consideration of diabetes and risk factors for comprehensive control of diabetic retinopathy.
These 10 causes are considered triggers and risk factors for the development of diabetic retinopathy
Diabetic retinopathy is caused by damage to the blood vessels in the retina due to diabetes mellitus. Here are the main causes of this eye disease in descending order of importance:
- Duration of existence of diabetes / diabetes: the longer diabetes exists, the higher the risk of diabetic retinopathy due to chronic vascular damage.
- Type 1 diabetes a male gender: Men with type 1 diabetes may have an increased risk of developing diabetic retinopathy.
- Poor control of blood sugar levels: Unregulated blood sugar levels favour damage to the blood vessels of the retina.
- Phases of hormonal change (puberty and pregnancy): Changes in hormones during puberty and pregnancy increase the risk of these retinal diseases.
- High blood pressure: High blood pressure damages the blood vessels in the retina and is one of the causes of diabetic retinopathy.
- Diabetic kidney damage: A damaged kidney increases the risk of eye diseases due to disturbed metabolic processes.
- Increase in blood lipids: Abnormal lipid metabolism levels can affect the blood vessels in the retina and favour a diabetic retinopathy diagnosis.
- Smoking: Smoking impairs blood flow to the small blood vessels in the eye and promotes inflammatory processes.
- Dry eyes: Reduced tear film stability can lead to an increased tendency to inflammation.
- Sunlight: Long-term exposure to intense sunlight, especially without suitable eye protection, can favour the risk of oxidative stress factors developing in the retina.
In addition to the diagnoses of macular degeneration (AMD), glaucoma, retinal degeneration and retinitis pigmentosa, diabetic retinopathy is one of the degenerative eye diseases.
A recommendation for patients
If you suffer from diabetes, it is important to keep an eye on your eye health. Watch out for possible symptoms such as deteriorating vision, distorted vision or flashes in the field of vision.
Have a regular eye examination to recognise changes at an early stage.
Diagnostic methods such as optical coherence tomography (OCT) enable a precise assessment. Check your blood sugar and blood pressure to minimise the risk.
The various options for Diabetic Retinopathy treatment
Diabetic retinopathy treatment requires a holistic approach to slow down the disease. While a complete cure is not possible, there are options for stabilisation.
Here we emphasise the various treatment methods used in conventional medicine. These include measures such as weight reduction, physical activity, dietary changes and abstaining from alcohol. Continuous monitoring and regulation of blood glucose levels is particularly important in order to curb the progression of diabetic retinopathy.
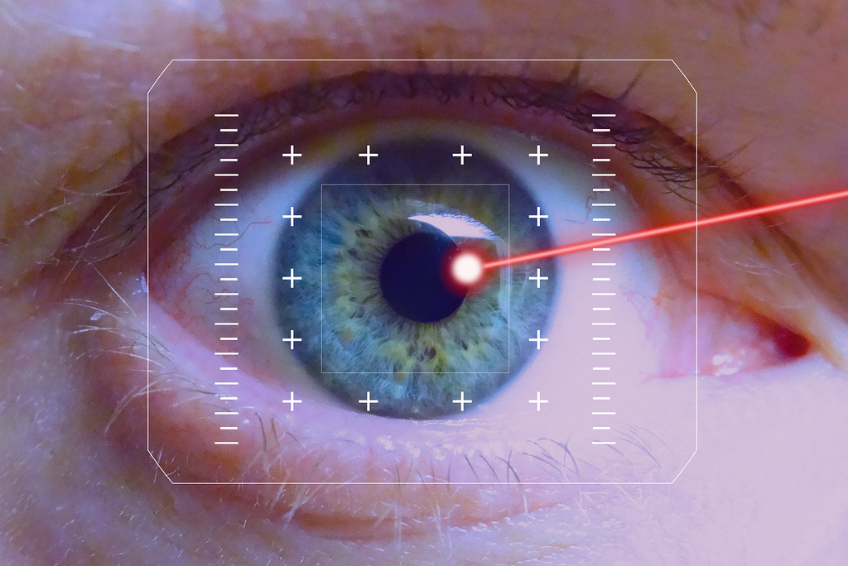
Laser therapy is a promising option in the early stages of the disease. Various laser treatments, including panretinal photocoagulation, focal laser therapy and laser-induced regression therapy, can be used depending on the stage and type of disease. Choosing the appropriate laser treatment requires consultation with an ophthalmologist.
In advanced stages of diabetic retinopathy, surgical procedures such as vitrectomy or photocoagulation may be considered. These procedures are usually considered when other measures are no longer sufficient.
Naturopathic approaches such as eye acupuncture, physiotherapy, vital substance therapy and dietary changes can also have a supportive effect. Early intervention and comprehensive care are crucial to maximise the chances of success in the treatment of diabetic retinopathy.