Angle-closure glaucoma treatment
Angle-closure glaucoma treatment – we provide a complete overview of the various treatment methods for angle-closure glaucoma
Angle-closure glaucoma, also known as pupillary block, is caused by sudden blockages in the outflow of aqueous humour. The most common cause of this blockage is a significant narrowing of the chamber angle through the iris. This condition can lead to a medical emergency.
The acute obstruction of the aqueous humour outflow leads to a rapid and drastic increase in intraocular pressure, often to three times or more the normal value. This can lead to values of up to 70 mmHg. Normally only one eye is affected by angle-closure glaucoma.
This is a medical emergency that requires immediate ophthalmological intervention, otherwise there is a risk of irreparable damage to the optic nerve.
It is crucial to carefully examine the affected eye and, if necessary, take precautionary measures in the other eye, as the anatomical conditions of both eyes are usually very similar.
It is worth noting that certain medications, especially drugs with an anticholinergic effect such as antiemetics or certain antidepressants, can increase the risk of angle-closure glaucoma. A detailed medical history and regular ophthalmological check-ups are therefore important in order to identify possible risk factors.
Acute angle-closure glaucoma is characterised by
- Severe eye pain
- Reddening of the eye
- Reduced visual acuity or sudden loss of vision
- Coloured halos around light sources
- Headaches
- Nausea and vomiting
- Very hard eyeball
- Delayed or complete cessation of pupillary reflex (so-called light rigidity)
cardiac arrhythmia
The intraocular pressure is increased in such cases. Immediate treatment with local and systemic medication is necessary to prevent permanent loss of vision. As a definitive measure, an iridotomy is usually performed.
Pathophysiology of angle-closure glaucoma or acute glaucoma attack
Occlusion of the chamber angle can be primary in its cause, whereby the exact reasons are unknown, or secondary, which means that it is a consequence of another disease.
The occlusion can occur in acute, subacute (periodically occurring) or chronic form.
Diagnosis of angle-closure glaucoma
The diagnosis of acute angle-closure glaucoma is usually made by clinical examination and measurement of intraocular pressure (IOP). Due to corneal opacities and fragile corneal epithelium, gonioscopy in the affected eye can be difficult.
However, an examination of the fellow eye can show whether there is a narrow or blocked angle. If the fellow eye has a normal angle, alternative diagnoses other than primary angle-closure glaucoma should be considered.
The diagnosis of chronic angle-closure glaucoma is based on the presence of peripheral anterior synechiae on gonioscopy and characteristic changes in the optic nerve and visual field as described in symptoms and complaints of primary open-angle glaucoma.
- Acute, primary angle-closure glaucoma: Diagnosis is based on measurement of intraocular pressure (IOP) and clinical findings.
- Chronic, secondary angle-closure glaucoma: In this form, gonioscopy reveals peripheral anterior synechiae and typical abnormalities in the optic nerve and visual field.
Acute, primary angle-closure glaucoma
Narrow aqueous angles are normally rare in the young population. With advancing age, however, the lens grows continuously. In some individuals, but not all, this lens enlargement will cause the iris to be pushed forward, resulting in a narrowing of the angle of the chamber.
Risk factors for developing a narrow chamber angle include:
People of Asian and Inuit descent have a higher risk, while the risk is lower in people of European and African descent.
A narrow chamber angle also means that the distance between the iris in the pupil area and the lens is very small. When the iris dilates, it is pulled centripetally (inwards) and comes into greater contact with the lens.
This can impede the flow of aqueous humour between the lens and the iris, preventing it from flowing through the pupil into the anterior chamber. This mechanism is known as “pupillary block”. Due to the pressure caused by the continuous production of aqueous humour in the ciliary body in the posterior chamber of the eye, the periphery of the iris is pushed forwards, resulting in a narrowing of the chamber angle.
This occlusion blocks the outflow of aqueous humour and leads to a rapid increase in intraocular pressure (> 40 mmHg) within hours.
Due to its rapid onset, this condition is referred to as primary acute angle-closure glaucoma. It is an ophthalmological emergency that requires immediate treatment.
There are also non-pupillary block mechanisms, such as plateau iris syndrome, in which the central anterior chamber is deep but the peripheral anterior chamber is flattened by a forward displaced ciliary body.
Intermittent angle-closure glaucoma occurs when episodic pupillary block occurs for a few hours and then resolves spontaneously, often after supine sleep.
The intraocular pressure rises only slowly in such cases. Chronic angle-closure glaucoma develops slowly as the chamber angle gradually closes and scarring may occur between the peripheral iris and the trabecular meshwork.
In patients with a narrow chamber angle, the dilation of the pupils (mydriasis) can push the iris into the chamber angle and trigger acute angle-closure glaucoma. This development is particularly relevant when topical drugs are used to dilate the pupils (e.g. cyclopentolate, phenylephrine) for examinations or for treatment (e.g. homatropine).
Or when systemic drugs are administered that have the potential to dilate the pupils (e.g. scopolamine, alpha-adrenergic agonists often used to treat urinary incontinence, or drugs with anticholinergic properties).
Symptoms and complaints of acute, primary angle-closure glaucoma
Patients with acute angle-closure glaucoma usually experience intense eye pain, reddened eyes, reduced visual acuity and coloured rings around light sources.
These symptoms are often accompanied by headaches, nausea and vomiting. The systemic symptoms can be so severe that a neurological or gastrointestinal problem is mistakenly diagnosed.
Typical clinical examination findings include reddened conjunctiva, a cloudy cornea, a fixed, moderately dilated pupil and signs of inflammation in the anterior chamber of the eye.
Visual acuity is reduced and the measured intraocular pressure (IOP) is usually between 40 and 80 mmHg. Due to corneal oedema, the optic nerve is difficult to see.
Due to the impaired general condition, visual field examination is usually not performed. If primary mechanisms of narrow-angle glaucoma, such as pupillary block or plateau iris, are suspected, examination of the unaffected eye can contribute to the diagnosis.
Treatment of acute, primary angle-closure glaucoma
The treatment of acute angle-closure glaucoma requires immediate action, as vision can be quickly and permanently jeopardised. The patient should be given various medications immediately.
The response to treatment is assessed by measuring the intraocular pressure (IOP). Miotics such as pilocarpine are generally no longer effective if the IOP is above 40 or 50 mmHg, as the pupillary sphincter is ischaemic and no longer responds.
Definitive therapy involves peripheral laser iridotomy, which creates an alternative outflow pathway for the aqueous humour from the posterior to the anterior chamber and resolves the pupillary block. This procedure is performed as soon as the cornea is clear and the inflammation has subsided. D
n some cases, the cornea can be cleared within hours of the IOP being lowered, while in other cases it may take 1-2 days. As the risk of an acute attack in the other eye is 80%, peripheral laser iridotomy is performed on both eyes.
Compared to the advantages of peripheral laser iridotomy, the risk of complications is extremely low, although discomfort such as glare (double vision) may occasionally occur.
Chronic, secondary angle-closure glaucoma
Mechanical blockage of the chamber angle occurs due to a concomitant disease such as proliferative diabetic retinopathy (PDR), ischaemic central retinal vein occlusion, uveitis or epithelial ingrowth.
Contraction of a neovascular membrane (e.g. in PDR) or inflammatory scarring can cause the iris to be pulled into the chamber angle. This leads to secondary angle-closure glaucoma.
Symptoms and complaints of chronic, secondary angle-closure glaucoma
Chronic angle-closure glaucoma is similar in appearance to open-angle glaucoma. Some patients complain of the typical glaucoma symptoms of red eyes, visual disturbances, discomfort or headaches. These symptoms often decrease during sleep, possibly due to the constricted pupil during sleep and the associated displacement of the lens by gravity.
A gonioscopic examination of the chamber angle reveals a constriction and peripheral anterior synechiae (adhesions between the peripheral iris and the angle structures blocking the trabecular meshwork and/or the ciliary body surface) may be visible. The intraocular pressure (IOP) may be normal but is usually elevated in the affected eye.
Treatment of chronic, secondary angle-closure glaucoma
In patients suffering from chronic, subacute or intermittent angle-closure glaucoma, peripheral laser iridotomy is also a recommended treatment option.
In addition, peripheral iridotomy should be considered immediately for narrow angle closure, even in the absence of symptoms, to prevent the development of angle closure glaucoma.
If a cataract is present, removal of the cataract can significantly slow the progression of chronic angle-closure glaucoma.
Drug and surgical treatment is largely the same as for open-angle glaucoma. However, it should be noted that a chamber angle that is so narrow that further anterior synechiae could occur after laser treatment is a relative contraindication for laser trabeculoplasty.
As a rule, non-penetrating lamellar surgery is not indicated in such cases.
Individualised care for angle-closure glaucoma – Integrated eye therapy according to Noll
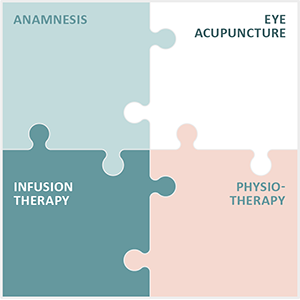
Angle-closure glaucoma is a particular challenge in ophthalmological care. In our practice, Augenakupunktur Noll, we have specialised in the individualised treatment of this and other chronic and degenerative eye diseases through the development of Integrated Eye Therapy according to Noll.
We offer our patients a deep understanding of the complexity of such diseases:
- An in-depth medical history to gain a complete picture of the health situation.
- Eye acupuncture according to Prof Boel, which serves as the central pillar of our treatment methodology.
- Customised infusion therapies that are specifically tailored to the needs and deficits of the individual.
- Specialised physiotherapy tailored to the patient’s specific eye problems.
Eye acupuncture according to Prof John Boel plays a key role in our therapeutic programme and is complemented by the three other pillars of our Integrated Eye Therapy according to Noll. Within 13 years, we have succeeded in building up an international patient base that reflects the trust in our method. We greatly appreciate the feedback from our patients, which motivates us to continue on our path of continuous improvement.
Although angle-closure glaucoma treatment is a serious and time-critical matter that often requires swift action, we understand the importance of a level-headed and holistic approach to therapy.
Each treatment is planned and carried out on the basis of a comprehensive diagnosis and taking into account the individual circumstances of our patients. Our aim is to contribute to the stabilisation and possible improvement of the situation with the utmost care and expertise, always within the framework of the possibilities offered by current research and our many years of experience.