Medication for glaucoma treatment
Cannabis is also a medicine for treating glaucoma. The use of cannabis for glaucoma treatment has been investigated in numerous studies
The aim of glaucoma treatment with medication
The basis of glaucoma treatment is to lower the intraocular pressure, both in the case of elevated intraocular pressure values and normal pressure glaucoma. Normal-tension glaucoma is a form of glaucoma in which the intraocular pressure is not elevated, but damage to the optic nerve still occurs.
The serious consequences of this disease can be prevented by initiating appropriate treatment in good time.
Treatment is aimed at lowering intraocular pressure and involves various approaches, including topical eye drops, oral medications, laser procedures and surgical interventions. In this form of the disease, therapy often begins with the application of suitable topical preparations to reduce the production of aqueous humour.
Different groups of medication in glaucoma treatment
Various groups of medications are used in the drug therapy of glaucoma, including acute glaucoma cases. These groups are aimed at improving the outflow of ocular fluid or reducing the production of fluid and are often used in combination.
The medication can be administered either topically in the form of eye drops or systemically. Here are some of the preparations and groups that are selected depending on the patient’s condition:
- Prostaglandin analogues
- Beta-blockers
- Alpha agonists (sympathomimetics)
- Carbonic anhydrase inhibitor
- Rho-kinase inhibitors
- Clofazoline
Prostaglandin analogues
These eye drops increase the uveoscleral oedema of the intraocular fluid, which leads to a reduction in the increased intraocular pressure. Popular representatives are latanoprost and bimatoprost.
Although effective, they can cause side effects such as eye redness, altered iris pigmentation, skin pigmentation changes on the eyelids and blurred vision.
Prostaglandin analogues should not be used in severe asthma, during pregnancy or breastfeeding and before eye surgery.
Beta-blockers
Drugs in this group reduce the production of ocular fluid by the ciliary body and thus lower the intraocular pressure. Commonly used preparations are timolol and betaxolol.
Side effects can include reddening of the eyes, blurred vision, bronchospasm, bradycardia and hypotension. Beta-blockers can also cause tiredness, drowsiness and depressive moods.
They are not suitable for patients with cardiovascular problems, respiratory diseases or allergies to the ingredients.
Alpha agonists (sympathomimetics)
These preparations reduce the production of ocular fluid and lower the intraocular pressure. Brimonidine and apraclonidine are sometimes used and can lead to local side effects such as redness, burning, itching, conjunctivitis and a foreign body sensation in the eye.
Systemic side effects may include an increase in blood pressure, cardiac arrhythmia, dry mouth and allergic reactions. Concomitant use with certain antidepressants is not recommended.
Carbonic anhydrase inhibitors
This group of drugs is used less frequently and includes preparations such as dorzolamide and brinzolamide. They inhibit the enzyme carbonic anhydrase in the ciliary body, which reduces the production of ocular fluid.
Carbonic anhydrase inhibitors are less effective and have a shorter duration of action compared to other medications.
They are more commonly used in acute glaucoma cases, usually systemically rather than topically. Side effects can include dryness and redness of the eyes, dermatitis, paraesthesia and depression.
Rho-kinase inhibitors
These medications, such as Rhokiinsa eye drops with the active ingredient netarsudil, were introduced in 2018. They reduce intraocular pressure in adults with open-angle glaucoma or ocular hypertension.
Netarsudil blocks the enzyme rho-kinase, which regulates the flow of fluid out of the eye. Rhokiinsa promotes the outflow of fluid from the eye and thus lowers the intraocular pressure.
The most common side effect is reddening of the conjunctiva. Other possible side effects are corneal curvature, pain when dripping and blurred vision.
Clofazolin
This medication is particularly effective in patients with high blood pressure, as it not only lowers systemic blood pressure but also reduces intraocular pressure.
Combined drug therapy for glaucoma
In general, we initially favour monotherapy with only one preparation in the treatment of glaucoma. However, if this does not have the desired effect, we resort to a combination of several active substances from different groups.
Combination preparations are often used here to relieve the patient and achieve an optimum effect. These combination eye drops contain two active ingredients that reduce eye pressure through complementary mechanisms.
The application is simple – one drop per day, either in the morning or in the evening. These innovative combination preparations expand our therapeutic options and make it possible to achieve the desired intraocular pressure and protect vision from damage.
One example of such a preparation is Simbrinza, which contains the active ingredients brinzolamide and brimonidine tartrate. Brinzolamide is a carbonic anhydrase inhibitor, while brimonidine tartrate is an alpha2-adrenoreceptor agonist.
These two substances work hand in hand to reduce intraocular pressure. Another preparation, Ganfort, contains bimatoprost and timolol, two active substances that also reduce intraocular pressure. Bimatoprost belongs to the group of prostamides, a prostaglandin analogue, while timolol is a beta-blocker.
Drug therapy for glaucoma attacks
A glaucoma attack is an acute emergency in which the intraocular pressure rises rapidly, often to values above 35 mmHg, in severe cases even up to 50-60 mmHg. This leads to characteristic symptoms within a few hours:
- Blurred vision
- Reddened eyes
- Lacrimation
- Swelling of the cornea, which becomes cloudy like “fogged glass”
Those affected see coloured rings or a rainbow halo around light sources. In severe cases, this can lead to loss of vision.
An attack of glaucoma requires immediate medical treatment by an ophthalmologist. Conservative therapy is aimed at lowering the intraocular pressure by opening the chamber angle and restoring the outflow of intraocular fluid.
Treatment often begins with 1% pilocarpine solution dripped every 5 minutes for half an hour, then every hour until the intraocular pressure drops. In addition, 1-2 tablets of acetazolamide are administered. If necessary, glycerine can also be administered orally. In some cases, tranquillisers and painkillers are required.
Preservative-free glaucoma preparations and their importance
In recent years, the range of drug therapy options for glaucoma patients has undergone a welcome expansion, particularly with the introduction of preservative-free preparations.
This is because in some patients, the preservative contained in eye drops triggers a so-called “sicca” problem or even exacerbates an existing tear film disorder.
Fortunately, almost all common classes of active ingredients are now available in preservative-free form, whether in single doses or other dosage forms that do not contain benzalkonium chloride – the most commonly used preservative in ophthalmology.
This development undoubtedly marks a milestone, particularly because preservative-free prostaglandins are now also available.
Bimatoprost as well as Tafluprost and Latanoprost are available in single-dose containers. Preservative-free combination preparations such as bimatoprost plus timolol are also available.
It is not only advisable to avoid preservative-free preparations for patients with sensitive eyes, dryness or a tendency to inflammation. As it is never possible to predict whether pressure-lowering surgery may be required in the future, the decision to avoid benzalkonium chloride is a proactive one.
This is because the ability of the conjunctiva to heal after such an operation could be impaired by years of exposure to this preservative. For patients with glaucoma and dry eye, the use of a preservative-free tear substitute is also recommended to supplement therapy.
Various options are available here, either in single-use doses or in special vials that do not require preservatives, such as those containing the disaccharide trehalose.
Possible side effects of glaucoma treatment with medication
The effect of glaucoma medication is to preserve vision. However, they can also have undesirable side effects. Some of these possible side effects are:
- A stinging or itchy sensation in the eyes
- Red eyes or reddened skin around the eyes
- Palpitations
- Increased blood pressure
- Potency problems
- Changes in breathing – especially in people with asthma or other breathing problems
- Dry mouth
- Blurred vision
- Changes in eye colour, the skin around the eyes or the eyelids.
If side effects of glaucoma medication are noticed, it is important to discuss these with your ophthalmologist. However, glaucoma medication should never be changed or discontinued without first consulting an ophthalmologist.
If the glaucoma does not respond to the medication or side effects cannot be tolerated, the doctor may recommend a change in medication or an operation.
Glaucoma medication during pregnancy: safety and risks
Before starting or continuing treatment during pregnancy, it is crucial to determine the procedure together with the woman concerned and to define the target intraocular pressure on the basis of existing findings.
As a rule, pregnancy has no significant effect on intraocular pressure and women with glaucoma can be reassured if they wish to have children.
In certain cases, however, temporary discontinuation of glaucoma medication in the first trimester may be considered, especially if the optic nerve is healthy and the intraocular pressure is not extremely elevated.
With regard to beta-blockers, epinephrine, apraclonidine, carbonic anhydrase inhibitors, parasympathomimetics and prostaglandin derivatives during pregnancy, there are official guidelines for categorisation as follows:
- Safety in pregnancy is uncertain
- No study results in humans are available
Only brimonidine is classified as probably safe based on animal studies.
Particular caution is required, especially in the first trimester, as all topical eye drops can cross the placenta.
Beta-blockers can cause cardiac arrhythmias and bradycardia in the foetus and are transferred into breast milk during breastfeeding.
Metipranolol has been shown to have a foetotoxic effect in the second and third trimester.
Prostaglandin derivatives can accelerate foetal development and lead to premature births.
Brimonidine should be discontinued before birth as it can lead to hypotension, sedation and even life-threatening respiratory distress in the newborn.
Carbonic anhydrase inhibitors, especially in systemic form, can cause severe electrolyte disturbances in the foetus and are possibly teratogenic in the first trimester.
Glaucoma treatment with cannabis
The use of cannabis to alleviate glaucoma symptoms has been investigated in numerous studies, and although some positive results have been obtained, doubts remain about its efficacy and consistency.
Nevertheless, it is one of the main reasons why people demand medicinal cannabis. We take a closer look at the research findings and the limitations of cannabis as a treatment option for glaucoma compared to conventional drug therapy.
The potential efficacy of cannabis in lowering intraocular pressure was first recognised in the 1970s. Pharmacologist Prof Manley West and his colleague, ophthalmologist Dr Albert Lockhart, published reports on the use of cannabis for glaucoma treatment in 1978.
West developed cannabis-based eye drops called “Canasol” for the treatment of glaucoma. In 1987, he received authorisation to market Canasol in Jamaica. Canasol contains no psychoactive cannabinoids and has reportedly been prescribed in various countries around the world, although it is only authorised in Jamaica. West later developed “Cantimol,” a combination of Canasol and the beta-blocker Timolol Maleate.
The effect of cannabis on intraocular pressure has thus been researched since the 1970s, but the medical community has not yet fully accepted cannabis as a treatment for glaucoma. A major reason for this is concerns about dosage and potential side effects.
The medical community is hesitant
Although cannabis can lower intraocular pressure, there are some challenges with its use as a glaucoma treatment. The effect of cannabis on intraocular pressure is short-lived, requiring frequent and high dosing to achieve a significant effect.
Patients would need to take around 18 to 20 mg of THC six to eight times a day to keep intraocular pressure in the normal range. This leads to considerable impairments in daily life, as side effects such as sleep disorders, mood swings and psychological problems can occur.
Another challenge is that tolerance to the intraocular pressure-lowering properties of cannabis could develop.
However, one study showed that long-term cannabis users still had lower intraocular pressure levels than non-users, even after a break of 3 to 10 hours before testing.
Treatment with cannabidiol (CBD) versus tetrahydrocannabinol (THC)
Cannabidiol (CBD) has gained popularity in recent years, but it is important to note that CBD does not have the same intraocular pressure-lowering properties as THC.
In fact, studies have found that CBD does not lower intraocular pressure and may cause a temporary increase. It may also interfere with THC’s ability to lower intraocular pressure.
The advantages and disadvantages of glaucoma treatment with cannabis at a glance
Advantages of cannabis therapy:
- Cannabis therapy offers a rapid effect, good tolerability and multiple benefits from a well-matched preparation.
- It is characterised by the absence of toxicity in cannabis products, is highly effective and is virtually free of side effects.
- In addition, the known neuroprotective effect of cannabis is considered a potential protection against progressive damage to the optic nerve.
Disadvantages of cannabis therapy:
- A disadvantage of cannabis therapy is the limited duration of the pressure-lowering effect.
- The short-term effectiveness requires frequent applications.
- The procurement and supply of medicinal cannabis is often difficult, and the different forms of administration can make access difficult for patients.
Access to medicinal cannabis for glaucoma patients
In some countries and regions, access to medicinal cannabis for glaucoma patients is regulated by law. These patients can obtain cannabis on medical prescription.
It is important to consult a specialist doctor who has experience with cannabinoid therapy. General practitioners, private doctors and other specialists can prescribe medicinal cannabis at the patient’s expense if this is appropriate according to the applicable laws and guidelines.
In South Tyrol, Italy, the ophthalmology departments of hospitals and other territorial institutions are listed as specialist centres for the prescription of medicinal cannabis.
Patients with glaucoma always have the possibility to consider this therapeutic option to improve their health.
Outlook for medicinal treatment with cannabis
Research into endocannabinoid mechanisms related to intraocular pressure has sparked interest in the development of cannabinoid-based glaucoma medications.
These drugs could significantly improve glaucoma treatment by providing neuroprotective, vasodilatory, antioxidant and anti-inflammatory properties in addition to lowering intraocular pressure.
Such new therapies could be particularly beneficial for patients who develop glaucomatous optic neuropathy despite normal intraocular pressure. Provided they are supported by high-quality clinical trials, they could represent an innovative and effective treatment option for glaucoma.
Regular medical follow-up for glaucoma drug treatment
Glaucoma is a serious disease and one of the leading causes of blindness. Preventing the progression of the disease is a common challenge. Regardless of its form, glaucoma leads to irreversible vision loss.
Therefore, regular check-ups and careful screening are essential to detect the disease early, control intraocular pressure and prevent severe damage to the optic nerve.
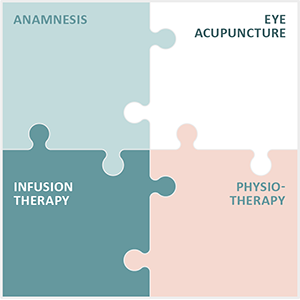
Integrated Eye Therapy according to Noll: Holistic treatment of chronic eye diseases
Noll Eye Acupuncture specialises in the treatment of chronic and degenerative eye diseases. The customised Integrated Eye Therapy according to Noll, developed by Michaela Noll, combines four essential elements into a holistic treatment concept:
- An extensive medical anamnesis: A detailed initial examination to understand the specific needs of each patient.
- Eye acupuncture according to Prof Boel: A central element of the therapy based on the individual diagnosis.
- Customised infusions: Tailor-made for specific nutritional needs and health conditions.
- Specialised physiotherapy: To support physical eye functions.
In more than 13 years of existence, the practice has not only built up an international patient base, but is particularly proud of the many positive feedbacks from patients after treatments. This integrated treatment approach allows patients to receive both symptomatic and causal therapies tailored to their specific conditions.