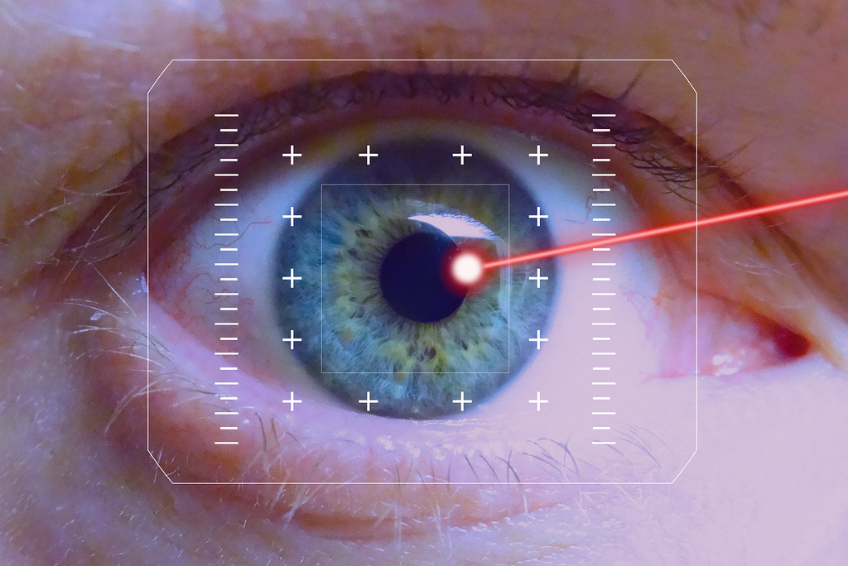
These are the 10 most important Diabetic Retinopathy causes and risk factors
The main cause of the development of Diabetic Retinopathy lies in the effects of prolonged elevated blood sugar levels on the small blood vessels in the retina.
These vascular changes can lead to damage to the retinal structures and impair vision in the long term.
These are the most common causes and risk factors for Diabetic Retinopathy in scientific research and in the everyday practice of Augenakupunktur Noll at a glance:
Duration of existence of diabetes is one of the most important Diabetic Retinopathy causes
The pathophysiological basis of Diabetic Retinopathy lies in the chronic hyperglycaemia associated with the prolonged course of diabetes. The persistently elevated blood glucose levels cause oxidative stress reactions, endothelial dysfunction and inflammatory processes in the retinal vessels.
These changes lead to structural abnormalities of the retinal microvasculature, especially the capillaries, which results in impaired blood supply to the retina. The progressive damage to the retinal vessels due to prolonged hyperglycaemia is thus a crucial catalyst for the development and progression of Diabetic Retinopathy.
Type 1 diabetes and a male gender
In type 1 diabetes, male gender has been identified as a risk factor for the development and progression of Diabetic Retinopathy.
Men with type 1 diabetes have an increased risk of developing Diabetic Retinopathy or a more severe form of the disease compared to women. This gender difference in susceptibility could be due to genetic, hormonal or other biological factors that may play a role in the development of diabetes complications.
The mechanisms behind this gender-specific association are not yet fully understood and further research is needed to clarify the exact links.
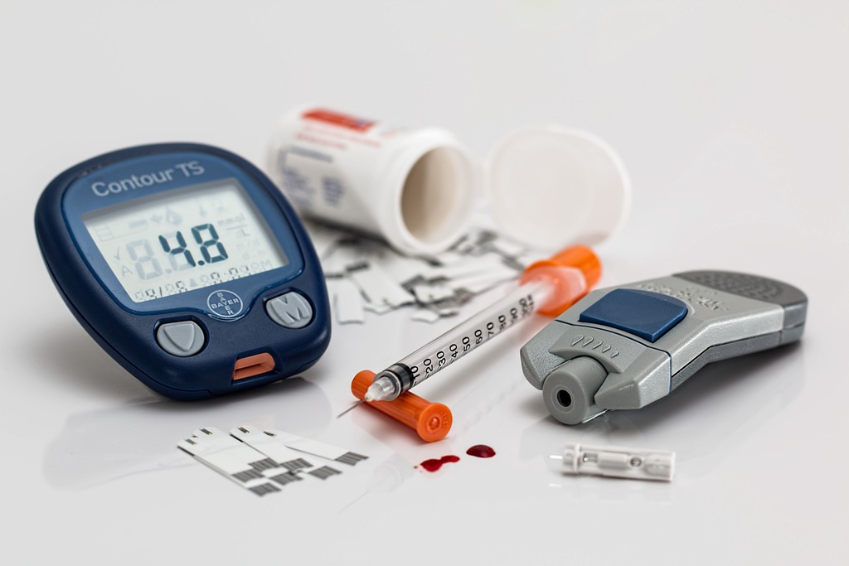
Poor control of blood glucose levels

Diabetics who do not adequately control and adjust their blood sugar levels run an increased risk of Diabetic Retinopathy
Diabetics who do not adequately control and adjust their blood glucose levels are at increased risk of Diabetic Retinopathy
Inadequate control of blood glucose levels is a significant factor in the development of Diabetic Retinopathy. If blood glucose levels are not well controlled over a long period of time, this can lead to oxidative stress and metabolic disorders.
These changes negatively affect the blood vessels in the retina and can lead to damage and changes in the vascular structure. Therefore, poor glycaemic control is a major contributor to the development and worsening of Diabetic Retinopathy as it exacerbates the negative effects of elevated glucose levels on the retinal microcirculation.
Phases of hormonal change (puberty and pregnancy)

Phases of hormonal changes such as puberty or pregnancy also increase the risk of developing or worsening Diabetic Retinopathy
Phases of hormonal changes such as puberty or pregnancy also increase the risk of developing or worsening Diabetic Retinopathy
During phases of hormonal changes such as puberty and pregnancy, there is an increased risk of developing and worsening Diabetic Retinopathy. These hormonal fluctuations can affect metabolism and blood flow, which can have a negative impact on the blood vessels in the retina.
In pubescent adolescents and pregnant women, these changes can contribute to Diabetic Retinopathy progressing faster or worsening. The risk of retinal complications can be increased during these phases, especially if blood sugar is insufficiently controlled and blood pressure is elevated.
High blood pressure
High blood pressure, also known as hypertension, plays a significant role as an independent risk factor in the development and worsening of Diabetic Retinopathy.
Like the other causes and risk factors, this leads to excessive strain on the blood vessels in the retina, favouring damage to the fine blood vessels that are necessary for the supply of the eye tissue.
The increased strain can lead to reduced blood flow to the retina and to constrictions in the vessels, which in turn disrupts microcirculation and impairs the integrity of the vessel walls.
The combined effect of diabetes and high blood pressure further exacerbates these negative effects. Both diseases contribute to vascular damage by triggering inflammatory processes and oxidative stress reactions in the body.
In diabetes in particular, the increased blood glucose level is a catalyst for vascular damage, while high blood pressure favours structural changes in the vessel walls. This combined effect leads to impaired vascular integrity and function, which can hereditarily increase the risk of Diabetic Retinopathy.
Given these links, controlling blood pressure in people with diabetes is of great importance to minimise the risk of Diabetic Retinopathy. Careful monitoring and treatment of high blood pressure can help to reduce the strain on the blood vessels and thus promote your long-term eye health.
Diabetic kidney damage (diabetic nephropathy)
Diabetic kidney damage, also known as diabetic nephropathy, is a significant cause of the development and progression of Diabetic Retinopathy.
This complication occurs due to long-term elevated blood glucose levels in diabetes and affects the function and structure of the kidneys. Chronic hyperglycaemia damages the small blood vessels in the kidneys, which leads to impaired kidney function.
Diabetic kidney damage favours the development of Diabetic Retinopathy through complex biochemical changes in the body. As a result of the impaired kidney function, there is a disturbed balance of body fluids, an increase in blood pressure and increased excretion of inflammatory and oxidative substances.
These factors contribute to a general tendency towards inflammation and damage to blood vessels throughout the body, including the retinal vessels.
The interaction between diabetic kidney damage and Diabetic Retinopathy exacerbates the pathophysiological process and worsens the microvascular environment in the eye. Impaired renal function leads to increased risks for inflammatory processes, oxidative stress and vasculopathy.
Overall, diabetic kidney damage underlines the complex nature of this eye disease and emphasises the importance of a comprehensive diabetes management strategy to protect both kidney function and eye health.
Increase in blood lipids
Cholesterol and triglycerides are considered an indirect Diabetic Retinopathy cause
The elevation of blood lipids, especially cholesterol and triglycerides, is a significant factor in the development and progression of Diabetic Retinopathy. High blood lipid levels are often associated with impaired metabolic function in diabetes, which affects various biochemical processes in the body. This can lead to damage to the blood vessels that supply the retina.
The increased blood lipid levels promote inflammatory reactions in the body, which leads to impaired vascular function. In the eyes, these changes can lead to damage to the blood vessels in the retinal wall and in the choroid. This damage impairs microcirculation in the eye and favours the development of microaneurysms, vascular leaks and haemorrhages in the retina.
The interaction between increased blood lipid levels and Diabetic Retinopathy exacerbates the negative impact on vascular integrity and contributes to chronic inflammation. The resulting changes in the blood vessels contribute to impaired nutrient supply to the retinal cells, which can ultimately lead to progressive vision loss.
Controlling blood lipid levels as part of comprehensive diabetes management is therefore crucial to minimise the risk of developing and progressing Diabetic Retinopathy.
Smoking
Smoking is one of the top ten Diabetic Retinopathy causes and risk factors
Smoking is a significant risk factor for the development and worsening of Diabetic Retinopathy. People with diabetes who smoke have an increased risk of developing Diabetic Retinopathy and experiencing faster progression of the disease.
Tobacco use is known to damage blood vessels and blood flow to the retina. Which can lead to a deterioration in eye health. The exact mechanisms by which smoking affects Diabetic Retinopathy are complex and could be due to inflammatory processes, oxidative stress and vasoconstriction.
Dry eyes
Dry eyes can occur when tear production is insufficient or the quality of the tear fluid is impaired. This condition can lead to discomfort and irritation of the eyes.
The exact relationship between dry eyes and Diabetic Retinopathy is complex. It is thought that inflammatory processes and metabolic changes associated with diabetes may also affect the ocular surface.
Adequate hydration of the eyes is important to minimise any potential impact on retinal health.
Sunlight
Intense sunlight can exacerbate the increased metabolic stress caused by diabetes
Exposure to intense sunlight is considered a possible risk factor for the development of Diabetic Retinopathy.
The ultraviolet rays in sunlight can cause oxidative damage to eye tissues, including the retina.
This oxidative stress can lead to inflammatory processes and exacerbate the metabolic stress already increased by diabetes.
Some studies emphasise the importance of adequate eye protection from excessive sun exposure, especially in people with diabetes, to minimise potential damage to the retina.
Consciously avoiding excessive sun exposure and wearing UV protective eyewear could help to reduce the risk of Diabetic Retinopathy.