Pigment dispersion syndrome treatment and pigmentary glaucoma treatment
Pigment dispersion syndrome treatment and pigmentary glaucoma treatment – we provide a complete overview of the various treatment methods
Pigment dispersion syndrome and pigmentary glaucoma
When pigment cells detach from the back of the iris and float in the aqueous humour of the eye, this is known in ophthalmology as pigment dispersion syndrome (PDS). If this condition remains untreated, it can develop into pigment dispersion glaucoma.
The development of this eye disease occurs when pigment cells are detached from the back of the iris and float freely in the aqueous humour of the eye. If the disease remains untreated, pigment cells can accumulate in the anterior chamber of the eye.
Here, these cells lead to blockage of the main site for the drainage of the aqueous humour, the so-called trabecular meshwork. As a result, the aqueous humour cannot drain properly and the intraocular pressure rises.
If only the PDS is present, there are initially only occasional increases in intraocular pressure. However, if the pressure is sufficiently high and persistent, this can lead to damage to the optic nerve. At this stage, ophthalmology speaks of pigment dispersion glaucoma (pigment glaucoma).
This is accompanied by a painless loss of vision. Early detection of the disease is crucial for further treatment.
Origin and risk factors of pigment dispersion syndrome and pigmentary glaucoma
The development of pigment dispersion syndrome (PDS) and later pigmentary glaucoma is most likely due to a concave structure of the iris. During the normal movement of the pupil, friction occurs between the posterior surface of the iris and the anterior lens of the eye.
This causes tiny pigment granules to be detached from the iris. Over time, these particles accumulate in the trabecular meshwork, which impedes the outflow of aqueous humour and increases intraocular pressure. This increased pressure inside the eye often leads to the development of pigmentary glaucoma.
This eye disease mainly affects European men between the ages of 25 and 40, especially those who are short-sighted. The progression of the disease usually ends around the age of 40, as the lens of the eye hardens at this point and there is no longer any contact between the iris and the lens.
It is assumed that genetic factors can favour the transition from the syndrome to glaucoma. It also appears that physical exertion, such as sport, can favour the development of the disease.
Symptoms of pigment dispersion syndrome and pigmentary glaucoma
People who suffer from PDS and pigmentary glaucoma often have myopia, and some families may have a history of glaucoma. Typically, symptoms of the syndrome are rare.
However, some patients may experience a so-called “pigment storm” after intense physical exertion, in which there is a massive release of pigment cells. This leads to
- A sudden increase in intraocular pressure
- Accompanied by visual disturbances, e.g. blurred vision
- And headaches
In advanced stages, when pigmentary glaucoma is already present and both eyes are affected, vision is reduced.
A specific symptom of pigment dispersion glaucoma are so-called rainbow circles that appear when looking into bright light. These circles are caused by deposits of melanin granules on the posterior corneal surface and are independent of intraocular pressure.
Determining the risk factors for the development of pigment dispersion syndrome and pigmentary glaucoma
In the diagnostic process, the potential risk factors should first be thoroughly considered, especially in the case of pre-existing PDS, in order to recognise the development of pigmentary glaucoma at an early stage and counteract it accordingly.
Reduced corneal thickness
Another risk factor for the development of glaucoma is a thinner cornea. Corneal thickness can be measured without contact. However, it is important to note that if the cornea is thicker, the intraocular pressure can be measured incorrectly high and if the cornea is thinner, it can be measured incorrectly low.
This means that the measurement of intraocular pressure alone is not a sufficient basis for a clear diagnosis.
A higher patient age
Glaucoma is more common in older people, but pigmentary glaucoma as a result of PDS can also affect younger patients. If changes in intraocular pressure and visual acuity occur, a diagnosis should be considered.
High intraocular pressure
Intraocular pressure plays a crucial role in the development of glaucoma, although there is no absolute value at which glaucoma is diagnosed. In ophthalmology, it is assumed that each eye can tolerate an individual internal pressure, which is referred to as the target pressure.
In pigment dispersion syndrome, the intraocular pressure can increase due to restricted aqueous humour outflow, thus favouring the development of glaucoma.
Goldmann applanation tonometry is the most accurate method for measuring intraocular pressure. It involves touching the anaesthetised cornea with a small measuring bulb and calculating the eye pressure based on the counterpressure exerted by the bulb.
A less precise method is the measurement with air blasts, in which the cornea is deformed and this deformation is measured with light and converted into the eye pressure. As intraocular pressure fluctuates throughout the day, regular 24-hour measurements are recommended.
Existing short-sightedness
Existing severe short-sightedness (from -5 dioptres) also increases the risk of pigmentary glaucoma. The link between short-sightedness and glaucoma lies in an unstable eye shell, which can cause damage to the optic nerve.
Low blood flow intensity
Insufficient blood flow to the optic nerve can favour the development of pigmentary glaucoma, and this can be influenced by high or low blood pressure.
Migraines or vascular spasms can indicate circulatory disorders.
A genetic predisposition
If there is a family history of PDS or pigmentary glaucoma, the risk of developing the disease increases.
The presence of sleep apnoea syndrome
Heavy snoring, accompanied by pauses in breathing, impairs the oxygen supply to the optic nerve and increases the risk of pigmentary glaucoma if PDS is already present.
A burden due to ethnic origin
Glaucoma is more common in people of African descent and has a more severe course. Pigmentary glaucoma, on the other hand, is more common in people of European descent.
However, it is more difficult to recognise iris defects due to the thicker, brown iris in people of African descent, so the exact prevalence of pigmentary glaucoma in this population is unclear.
Diagnosis of pigment dispersion syndrome and pigmentary glaucoma
The diagnosis of pigment dispersion syndrome and pigmentary glaucoma requires the use of various measurement methods, in particular for measuring intraocular pressure.
Biomicroscopy
Biomicroscopy uses a slit lamp to examine the fundus of the eye, in particular the optic nerve head and the nerve fibre layer, in more detail.
For a detailed assessment, eye drops are administered about 20 minutes before the examination to dilate the pupil. Suspicions of PDS or pigment dispersion glaucoma arise from the following findings:
- Spindle-shaped pigment deposits on the inside of the cornea (Krukenberg spindle).
- Significant pigment deposits on the iris surface and in the chamber angle.
- Defects in the iris in the form of slits (stained-glass window phenomenon).
The intraocular pressure is initially within the normal range, but increases and is often higher than in primary open-angle glaucoma. This indicates that the optic nerve is damaged more quickly.
The Heidelberg Retinatomograph (HRT)
The HRT is a laser scanner that can visualise the surface of the optic nerve head in three dimensions in the range of hundredths of a millimetre. This can reveal early changes in the optic nerve that are not yet visible with the slit lamp.
The examination is painless and non-contact, and pupil dilation is not required.
Optical coherence tomography (OCT)
OCT enables high-resolution visualisation of the various layers of the retina. This diagnostic procedure helps to identify damage to nerve fibres as part of the early detection of glaucoma.
The OCT examination is also non-contact and painless, but sometimes requires the pupil to be dilated beforehand.
Functional diagnostics
In functional diagnostics, examinations of colour vision and twilight vision are carried out. This makes it possible to recognise and classify certain retinal and optic nerve diseases.
The methods used in functional diagnostics include, for example
- The standard visual field measurement
- Blue-yellow perimetry
- Frequency doubling perimetry
Standard visual field measurement (also known as white-white perimetry)
In this method, bright points of light are projected alternately onto different parts of a hemisphere. The patient presses a switch in his hand when he perceives one of these points of light.
Each point of light corresponds to a specific spot on the retina of the eye. This measurement helps to determine whether there is already functional damage, as can occur with glaucoma.
Each eye is examined individually and the patient must direct their gaze to a fixed point in the centre of the hemisphere without following the points of light with their eyes.
Blue-yellow perimetry
In this method, a bright blue dot is projected onto a yellow illuminated hollow sphere. The examination is similar to the visual field measurement.
This method is well suited to younger patients without lens opacities and is more sensitive than white-white perimetry, which means that even slight visual field defects can be detected.
The examination requires a high level of concentration from the patient.
Frequency doubling perimetry
This method is similar to visual field measurement, but usually indicates damage at an earlier stage. Instead of points of light, a flicker strip pattern is used as a stimulus.
This technique makes it possible to recognise early signs of visual field changes and is particularly sensitive to glaucoma-specific defects.
Differential diagnoses to be considered in the context of pigment dispersion syndrome and pigmentary glaucoma
First of all: Differential diagnoses are diseases that have similar or almost identical symptoms and must therefore be considered by the doctor as potential causes of the patient’s symptoms in addition to the main suspected diagnosis.
The diagnosis of pigmentary dispersion glaucoma requires careful consideration of differential diagnoses to ensure accurate confirmation.
These four differential diagnoses should be considered in the diagnosis of pigmentary dispersion syndrome and pigmentary glaucoma:
- Presence of uveitis
- Presence of trauma or trauma
- Presence of pseudoexfoliation glaucoma
- Presence of overlap syndrome
Presence of uveitis
Uveitis is an eye disease in which the vascular membrane of the eye is inflamed. Involvement of the iris (iritis) in particular can cause symptoms similar to those of pigment dispersion glaucoma.
Slit lamp examination can detect abnormalities and inflammatory cells in the anterior chamber of the eye may indicate uveitis.
Presence of trauma or trauma
Eye injuries can lead to various symptoms, including blurred vision, similar to pigment dispersion glaucoma.
The typical changes in this disease and the medical history can help to rule out injuries.
Presence of pseudoexfoliation glaucoma
This condition mainly occurs in older people and leads to deposits in the drainage pathways of the eye and on the lens surface.
It can lead to an increase in intraocular pressure, but the symptoms are different from those of pigment dispersion glaucoma.
Presence of overlap syndrome
Overlap syndrome is characterised by symptoms or diagnostic features of at least two clinical pictures.
It often occurs in autoimmune diseases and can also affect the eyes, which can lead to a variety of symptoms, including uveitis. Treatment is focussed on alleviating the symptoms.
Treatment of pigment dispersion syndrome and pigmentary glaucoma
The treatment of pigment dispersion syndrome (PDS) and pigmentary glaucoma is challenging as there is no direct causative treatment.
The treatment approaches are essentially similar to those for primary open-angle glaucoma.
There are different approaches to control the increased intraocular pressure and to take potential risk factors into account:
Drug therapy
Drug therapy is often used as a first line treatment. Pilocarpine, a parasympathomimetic, was previously used as a treatment to reduce the concavity of the iris and lower intraocular pressure.
However, pilocarpine can cause side effects such as myopia and accommodative spasms, so newer drugs are now more commonly used, including beta-blockers, topical prostaglandins, carbonic anhydrase inhibitors and alpha-adrenergic agonists.
Prostaglandin analogues are popular as they promote the drainage of pigment from the trabecular meshwork. Regular check-ups every three to six months are important to monitor intraocular pressure and recognise early signs of glaucoma.
Surgical therapy
Surgical interventions can be considered for pigment dispersion syndrome and pigmentary glaucoma.
- Laser iridotomy: Laser iridotomy can create tiny holes in the iris to allow the drainage of aqueous humour. However, this minimally invasive procedure is considered more of a preventative measure.
- Argon laser trabeculoplasty (ALT) or selective laser trabeculoplasty (SLT): Argon laser trabeculoplasty (ALT) or selective laser trabeculoplasty (SLT) can reduce intraocular pressure in some cases, although their long-term effectiveness is not yet fully understood.
- Trabeculectomy: In more severe cases, a trabeculectomy may be necessary to create an artificial drain for aqueous humour.
The aim of the surgical measures
The main aim of surgical procedures is to permanently regulate intraocular pressure. Regular follow-up examinations are therefore crucial to monitor the success of the procedure.
Unfortunately, nerve damage that has already occurred due to increased intraocular pressure is often irreversible.
Possible complications of surgical procedures
Laser iridotomy can lead to a temporary increase in intraocular pressure in patients with PDS and pigmentary glaucoma, which can be avoided by using low energy levels and administering alpha-adrenergic agonists before and after treatment.
Trabeculectomy can lead to scarring, which can hinder the success of the procedure and lead to a renewed increase in intraocular pressure.
In such cases, a needling procedure can be performed to reduce scarring and improve aqueous humour outflow. If scarring persists, a repeat trabeculectomy may be required.
Prognosis for pigment dispersion syndrome and pigmentary glaucoma
The prognosis for patients with pigmentary dispersion syndrome is pigmentary dispersion glaucoma in about 30 per cent of cases. Despite this development, blindness is rare but not completely ruled out.
There is hope, however, as both pigment dispersion syndrome and pigmentary glaucoma can regress in some cases. There have even been documented cases of normalisation of pigmentation and iris transillumination defects.
Some patients with pigmentary glaucoma also experience an improvement in their intraocular pressure, possibly due to the cessation of pigment cell release.
The prognosis for these conditions can therefore vary, and early diagnosis and appropriate treatment are crucial for the long-term health of patients.
Preventing the development of pigment dispersion syndrome and pigmentary glaucoma
Prevention of pigmentary dispersion syndrome and pigmentary glaucoma focuses on reducing risk factors and regular screening to detect and treat the conditions early.
Here are some preventative measures:
- Regular eye examinations: Especially important for those at increased risk to detect changes early.
- Healthy lifestyle: A balanced diet, physical activity and controlling high blood pressure and diabetes all contribute to eye health.
- Smoking cessation: Smoking increases the risk of eye diseases, therefore smoking cessation is recommended.
- Eye protection: Take protective measures during hazardous activities to prevent injuries.
- Stress management: Stress can increase intraocular pressure, so use stress management techniques.
- Avoid impact: Patients are often advised to avoid sports such as martial arts or endurance running as they can cause impact, which can lead to detachment of pigment cells from the iris.
Genetic predisposition cannot be influenced, so regular screening and early diagnosis are crucial.
Advanced treatment concepts for pigment dispersion syndrome and pigment glaucoma at Augenakupunktur Noll
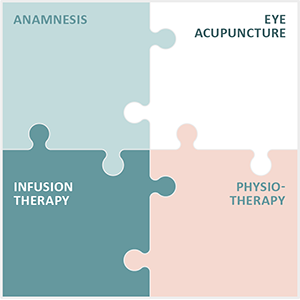
At Augenakupunktur Noll, we are dedicated to the treatment of chronic and degenerative eye diseases using the specialised and constantly refined Integrated Eye Therapy according to Noll, developed by Michaela Noll. This innovative therapy comprises:
- A comprehensive anamnesis, which serves as the cornerstone of every treatment
- Eye acupuncture according to Prof Boel, central to the therapy
- Individualised infusions, tailored to specific needs
- Targeted physiotherapy to support the healing process
For over 13 years, our practice has been a pioneer in treatment and research in the field of eye diseases and we are particularly proud of the positive feedback we have received from our international patient base.
Pigment dispersion syndrome and pigmentary glaucoma, in which pigment cells block the drainage channels of the eye and thus increase intraocular pressure, require early and precise diagnosis. Our Integrated Eye Therapy according to Noll uses advanced diagnostic procedures and personalised treatment strategies to address these challenges.
In our many years of practice, we have treated a large number of cases of pigment dispersion syndrome and pigmentary glaucoma, always focussing on individual patient care. The Integrated Eye Therapy according to Noll has proven to be useful in combining traditional and novel treatment methods.
Please note that each treatment is customised to the individual patient and results may vary. Regular monitoring and adjustment of therapy is essential to achieve the best possible outcome.