Retinitis Pigmentosa treatment – all options from retinal implants to complementary methods
Advances in ophthalmology offer a range of possibilities for the treatment of retinitis pigmentosa. From retinal implants that partially replace defective photoreceptors to gene therapy that works at the genetic level, new horizons are opening up.
Electronic visual aids and optical aids offer additional possibilities for improving quality of life. The targeted treatment of concomitant diseases such as cataracts and macular oedema as well as the inclusion of nutrition and dietary supplements round off the spectrum.
Retinal implants (retinal implant systems) or the subretinal retinal implant
Retinal implants, also known as retinal implant systems, are an advanced option for retinitis pigmentosa treatment. This innovative technology aims to improve the vision of patients suffering from progressive vision loss due to this degenerative eye disease.
How the retinal implants work
Retinal implants usually consist of a small electronic device that is surgically inserted into the eye. The implant partially replaces the function of the damaged photoreceptors, which are responsible for converting light into electrical signals.
In retinitis pigmentosa, these photoreceptors degenerate over time, leading to loss of vision.
The implant contains tiny electrodes that are placed directly on the surface of the retina. These electrodes are designed to stimulate the intact retinal ganglion cells, which normally transmit the signals from the photoreceptors.
This electrical stimulation generates impulses that are transmitted to the brain via the optic nerve and interpreted as visual perception.
Implantation process of retinal implants
The implantation of a retinal implant is a surgical procedure performed by an experienced eye surgeon.
During the procedure, the implant is carefully positioned on the retina and the electrodes are placed so that they come into contact with the still functioning cells. The accuracy of this placement is crucial to the success of the treatment.
After implantation, the patient needs a certain amount of time to get used to the new visual experience. Perception via the retinal implant may initially be different to normal vision and a period of adjustment is required.
Successes and challenges of retinal implants
Retinal implants have led to significant improvements in vision in some cases. Patients may be able to recognise light sources, distinguish outlines of objects or even see simple shapes.
However, individual response to this technology varies, and not every patient experiences the same results.
It is important to note that retinal implants are not equally effective for all forms of retinitis pigmentosa, and there are also some challenges. The number of electrodes and the limited resolution of vision are factors that can affect the level of detail.
In addition, potential complications can occur after implantation that require careful monitoring.
Final considerations for treatment with retinal implants
Deciding on a retinal implant as a treatment option requires a thorough evaluation of the individual’s medical condition and the specific characteristics of retinitis pigmentosa. Close collaboration with an experienced ophthalmologist is essential to weigh the pros and cons and discuss the patient’s realistic expectations.
This technology remains a promising approach to improving vision in people with retinitis pigmentosa, while further development and research in this area continues.
Transcorneal electrical stimulation (TES)
How transcorneal electrical stimulation (TES) works
Transcorneal electrical stimulation (TES) is a treatment option for people with retinitis pigmentosa (RP) that aims to stimulate the remaining cells in the retina.
Performing transcorneal electrical stimulation (TES)
The process of transcorneal electrical stimulation involves the placement of electrodes on the cornea of the eye. These electrodes generate electrical impulses that travel through the cornea to the cells of the retina.
The electrical signals are intended to stimulate the preserved retinal cells to induce visual perceptions.
The treatment is usually performed on an outpatient basis and does not require any invasive surgical procedures. The electrodes can be placed temporarily on the cornea and treatment sessions can be repeated regularly to achieve the desired effects.
Successes and challenges of transcorneal electrical stimulation (TES)
Transcorneal electrical stimulation has shown promising results in several studies. Patients who have undergone retinitis pigmentosa treatment have reported improved light sensitivity, enhanced peripheral vision and better perception of contrast.
It is important to note that results can vary from person to person, and not all patients experience the same improvements.
Challenges of this method include the limited spatial resolution of the induced perceptions and the fact that the effects may diminish after treatment sessions. Here too, long-term efficacy and safety are still the subject of further research.
Gene therapy as an option for retinitis pigmentosa treatment
How gene therapy works
Gene therapy is a promising approach for the treatment of retinitis pigmentosa, a genetic eye disease. The aim of this therapy is to correct or replace the defective genes responsible for the disease.
In retinitis pigmentosa, genetic mutations cause the photoreceptors in the retina to die, leading to progressive vision loss.
In gene therapy, healthy copies of the defective gene are usually introduced into the cells of the retina. This can be done using various techniques, including the use of viruses as vectors that transport the genetic information into the cells.
The healthy genes are intended to restore the function of the photoreceptors and slow or stop the progression of the disease.
Carrying out gene therapy
Gene therapy for retinitis pigmentosa requires a precise and targeted approach. Firstly, the healthy gene is incorporated into a vector virus, which is then introduced into the affected cells of the retina. This can be done by injection directly into the eye.
After the injection, the healthy gene integrates into the DNA of the target cells and begins to produce the normal protein. In this case, the therapy aims to stimulate the production of proteins that are important for the health of the photoreceptors.
Successes and challenges of gene therapy
Gene therapy has shown promising results in preclinical and early clinical trials. Some patients have shown improvement or at least a slowing of disease progression.
However, it is important to note that gene therapy for retinitis pigmentosa is still in the experimental stage and further research and clinical trials are needed to confirm its safety and efficacy.
The challenges of gene therapy for retinitis pigmentosa include precision of gene delivery, durability of genetic correction and customisation to individual patient genetic variations.
Outlook and research
Research in the field of gene therapy for retinitis pigmentosa is progressing and work is ongoing to improve the technique and optimise results.
New insights into the genetic causes of the disease could lead to customised therapeutic approaches that are specifically tailored to the individual genetic profile of patients.
Final thoughts on gene therapy as a treatment option for retinitis pigmentosa
Gene therapy for retinitis pigmentosa is promising, but it is important to have realistic expectations as this therapy is still in development. Participation in clinical trials may be an option for patients who wish to benefit from this advanced treatment.
Other treatment options such as optical and visual aids and electronic visual aids
Optical aids and visual aids
Optical and visual aids are an important treatment option for people with retinitis pigmentosa. These include specially adapted spectacles, magnifying glasses and other optical devices designed to optimise existing vision.
Through targeted adjustments such as contrast enhancement and magnification, these aids can help to improve the perception of objects and allow patients greater independence in everyday life. Customised spectacles can also help to expand the peripheral field of vision.
The optimal optical aids are selected in close co-operation with ophthalmologists and specialists in order to meet individual needs and the course of the disease.
Electronic visual aids
This technology utilises electronic devices such as wearable cameras and computer chips to convert visual information into acoustic or tactile signals. This conversion enables patients to better orientate themselves and perceive objects in their environment despite the progressive loss of their natural vision.
The electronic visual aids serve as innovative support in everyday life by enabling those affected to recognise obstacles and better understand their environment.
Possible electronic visual aids are, for example
- OrCam MyEye: Wearable camera that uses AI to recognise printed text, faces and products and communicates information via a loudspeaker.
- eSight glasses: Electronic vision aids with high-performance camera that transmit live images to a screen in front of the user’s eyes, customisable for improved vision.
- Sunu Band: Wearable wristwatch with ultrasonic sensors that detect obstacles in the environment and provide feedback to the user via vibrations.
- IRISVision: Virtual reality glasses with a camera that allow the user to see the environment on a screen and customise it.
Treatment of concomitant diseases
As retinitis pigmentosa is already associated with a progressive loss of photoreceptors, concomitant diseases such as cataracts or macular oedema can also impair vision.
Targeted treatment of these concomitant diseases not only serves to preserve current vision, but also attempts to create the best possible conditions for improving quality of life and independence.
Early detection and adequate treatment of these concomitant diseases is therefore of crucial importance.
Treatment of concomitant cataracts
Surgery to remove the clouded lens and implant a clear intraocular lens to improve light transmission can be considered for cataracts. This operation can have a positive effect on visual acuity in the presence of retinitis pigmentosa.
Treatment of concomitant macular oedema
For macular oedema, which is often associated with inflammation, anti-inflammatory medication or, in some cases, injections into the vitreous of the eye may be considered to reduce the swelling and minimise the risk of further visual deterioration.
Complementary methods for retinitis pigmentosa treatment
Complementary treatments for retinitis pigmentosa include approaches such as acupuncture, homeopathy, nutritional optimisation and herbal supplements.
These methods aim to improve overall well-being, slow the progression of the disease and potentially improve vision.
Acupuncture can harmonise the energy flow in the body, homeopathic remedies are individually adapted.
A balanced diet rich in antioxidants and omega-3 fatty acids supports eye health.
Herbal supplements such as Ginkgo Biloba are sometimes discussed for their possible positive effects on circulation.
The importance of diet and supplements
Consideration of diet and supplements plays an important role in retinitis pigmentosa treatment. A balanced diet, rich in antioxidants, omega-3 fatty acids and vitamins, can help support retinal health and slow the progression of vision loss.
Specialised supplements, such as vitamin A, vitamin E and omega-3 fatty acids, are sometimes recommended to compensate for nutritional deficiencies and support photoreceptor function.
Eye Acupuncture Noll – Your partner in the treatment of retinitis pigmentosa
In modern ophthalmology, innovative ways of treating retinitis pigmentosa are constantly being researched and developed. In addition to established methods such as retinal implants and electronic visual aids, Noll eye acupuncture favours a holistic approach.
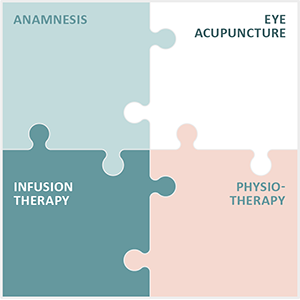
With the Integrated Eye Therapy according to Noll, a method finely tuned by Michaela Noll, we have been dedicated to the treatment of chronic and degenerative eye diseases for 13 years. Our approach includes
- a comprehensive anamnesis,
- precise eye acupuncture according to Prof. Boel,
- individually customised infusions
- and special physiotherapy to create a personalised treatment concept for each individual patient.
Eye acupuncture, as the centrepiece of our therapy, is supplemented by supportive measures that can increase well-being and positively influence the course of the disease.
Our extensive experience and the development of an international patient base testify to the trust placed in our practice and the success of our therapeutic approaches.