Glaucoma surgery
Glaucoma surgery: A distinction can be made between three types of surgery or laser treatment
Glaucoma can be treated with both glaucoma surgery and laser treatment. These options are considered if it is not possible to control the intraocular pressure with medication alone or if the drops are not well tolerated.
A distinction can be made between three types of surgery or laser treatment:
- Glaucoma surgery Trabeculectomy
- Laser treatment
- Minimally invasive surgery
Glaucoma surgery Trabeculectomy
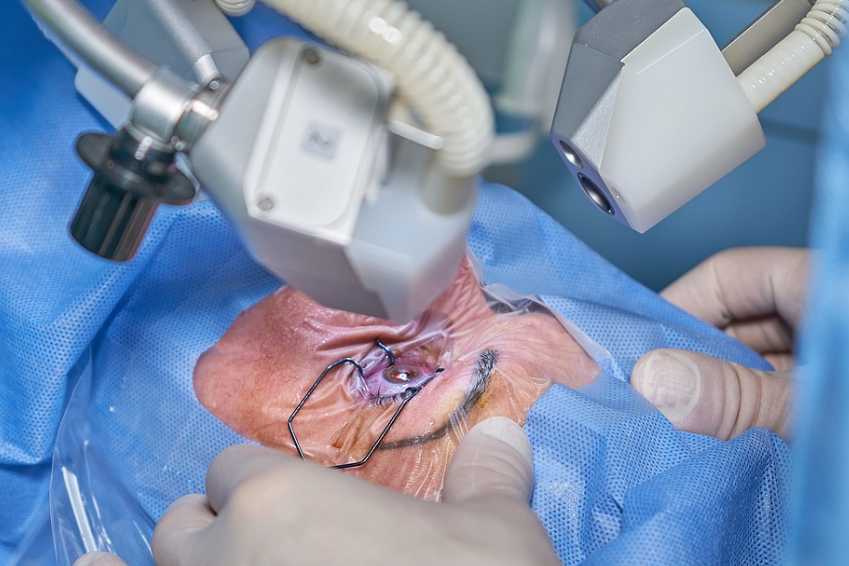
Glaucoma surgery has the long-term goal of permanently reducing intraocular pressure to low levels. The most common surgical method is trabeculectomy.
The surgeon cuts out a small piece of the sclera and the iris to improve the drainage of the aqueous humour and reduce the pressure in the eye.
Possible undesirable consequences of surgery include temporary visual disturbances, scarring and, in the long term, the development of cataracts.
Laser treatment
Laser treatment can also reduce intraocular pressure, but usually not as much as surgery.
Most laser procedures aim to improve the outflow of aqueous humour. There are also laser treatments that reduce the production of aqueous humour.
Laser treatment can be performed as an adjunct to eye drop therapy, but may have temporary side effects such as redness, dry eyes and temporary visual deterioration.
Two main types of laser surgery are available. These procedures are designed to facilitate the drainage of aqueous humour from the eye. Generally, these procedures are performed in an ophthalmologist’s office or in an outpatient surgery centre:
Laser trabeculotomy
A surgical procedure to reduce intraocular pressure in glaucoma. Laser trabeculotomy is a surgical procedure that is used in cases where the intraocular pressure is significantly too high and the optic nerve is already damaged.
In this glaucoma operation, the eye surgeon uses a laser to connect the drainage channel to the anterior chamber of the eye. This enables improved drainage of the aqueous humour from the eye and leads to a reduction in intraocular pressure.
Laser iridectomy
Laser iridectomy is a procedure in which the ophthalmologist uses a laser to create a tiny hole in the iris (the iris). This hole equalises the pressure between the anterior and posterior chamber of the eye, making it easier for the aqueous humour to flow into the drainage angle and out of the eye.
This procedure can help to reduce the intraocular pressure in glaucoma and thus control the progression of the disease.
Minimally invasive glaucoma surgery
Minimally invasive glaucoma surgery has been increasingly introduced in recent years. Small implants (stents) are inserted into the drainage canal to drain the aqueous humour and lower the intraocular pressure.
This procedure is usually offered to people with mild or moderate glaucoma. In most cases, minimally invasive procedures are not covered by health insurance if they are performed on an outpatient basis.
To date, there has been a lack of conclusive studies that have comprehensively analysed the advantages and disadvantages of the various minimally invasive methods in comparison to surgery or laser treatment.
Two minimally invasive surgical methods can be distinguished: Implants for glaucoma drainage and canaloplasty (360° canaloplasty)
Implants to promote glaucoma drainage
In some cases, your ophthalmologist can insert a tiny drainage tube into your eye to channel the aqueous humour to a reservoir. This reservoir is created under the conjunctiva and allows neighbouring blood vessels to absorb and drain the fluid.
Canaloplasty (360° canaloplasty)
Canaloplasty is a relatively new method in which a ring-shaped implant is permanently placed in Schlemm’s canal to keep it open and support drainage.
Indications for glaucoma surgery
In most cases, surgery is not the first choice for glaucoma treatment, but it can save your vision if other therapies are not effective.
Glaucoma surgery may also be considered if glaucoma medications are causing serious side effects such as increased blood pressure, palpitations or impotence.
In some patients, surgery may be necessary if the intraocular pressure is significantly too high and there is a risk to the optic nerve and therefore to vision.
Expectations of glaucoma surgery
Laser surgery to treat glaucoma can usually be performed in an ophthalmologist’s practice or in an outpatient eye surgery centre.
During the procedure, the eye is anaesthetised so that the patient feels little to no pain during the treatment. They may notice a slight stinging or burning sensation and may see a brief, bright flash.
Immediately after the operation, vision may be slightly blurred and the eye may feel a little irritated. The doctor will check the intraocular pressure a few hours after the operation. The patient should not drive themselves after the operation, but should be taken home by someone else.
It is recommended to rest at home for about a week. The patient should avoid driving, reading and lifting heavy objects. Direct contact of water or soap with the operated eye should be avoided.
The eye may be reddened, sensitive or slightly swollen. Vision may be slightly blurred for about six weeks. Contact lenses may only fit again after the swelling has subsided.
Around half of patients who undergo this operation no longer require medication to reduce intraocular pressure.
Glaucoma surgery procedure in general
Once glaucoma has been diagnosed, treatment with medication is usually initiated before glaucoma surgery is considered. The ophthalmologist will conduct a detailed preliminary consultation, even if he or she already knows the patient’s medical history.
During this consultation, the ophthalmologist will ask about the medication taken regularly, as certain preparations, such as blood thinners, must be temporarily discontinued.
He then discusses the appropriate form of anaesthesia with the patient. In most cases, glaucoma surgery is performed under local anaesthetic. The decision in favour of inpatient or outpatient surgery depends on the specific surgical procedure.
Glaucoma surgery varies in duration depending on its complexity and can take between 15 and 90 minutes. If both eyes are affected by glaucoma, the more severely affected eye is usually operated on first, followed by surgery on the second eye after a few weeks. This staggered procedure minimises the patient’s everyday impairments.
What to consider after glaucoma surgery: rest and medication
After glaucoma surgery, it is extremely important that the patient takes it easy physically for a few weeks. The prescribed eye drops should be used conscientiously and regularly, as the success of the treatment depends on this.
It is equally important that the patient avoids rubbing the eyes to prevent possible complications. If symptoms such as impaired visual acuity, bleeding or pain occur after the procedure, the patient should not hesitate to contact the treating ophthalmologist immediately.
Risks and chances of success of glaucoma surgery
The risks of glaucoma surgery vary greatly and depend on the condition of the eye before the procedure and the technique used. The doctor will provide detailed information about rare complications such as infections, problems with wound healing, visual field loss or post-operative bleeding before the patient can decide in favour of the procedure.
The success of the operation also depends on thorough aftercare, which is why regular follow-up appointments are crucial.
It is important to note that damage to the optic nerve and retina that has already occurred cannot be reversed by the operation.
The aim of the operation is to preserve existing vision. If there is no noticeable improvement in vision after the procedure, this should not be considered a failure of the operation.
Surgery to treat glaucoma can increase the risk of developing cataracts later on. Other possible risks may include
Eye pain or redness
- Persistence of too high or too low intraocular pressure
- Loss of vision
- Infection
- Inflammation
- Bleeding in the eye
Treatment of glaucoma and cataracts in a combined operation
Patients are increasingly affected not only by glaucoma, but also by cataracts. This is due to the increasing age of the population, as these diseases predominantly occur in old age.
As life expectancy increases, people are getting older, which leads to an increase in the number of diagnoses of “glaucoma” and “cataract”. In cataracts, the lens of the eye becomes cloudy over time due to tissue changes, which means that less and less light reaches the retina. If left untreated, this also leads to blindness.
Fortunately, both glaucoma and cataracts can be treated:
- Glaucoma is treated with medication, surgery or laser treatments to reduce intraocular pressure.
- Cataracts, on the other hand, are always treated surgically. During cataract surgery, the surgeon replaces the clouded lens of the eye with an artificial lens.
Choosing the right treatment makes it possible to preserve the patient’s eyesight in the long term.
Combined surgery for glaucoma and cataracts
Normally, glaucoma and cataracts are treated independently of each other. Under certain circumstances, however, it is possible to treat both diseases in a single operation.
This usually begins with a conventional cataract operation: the surgeon opens the eye with a small incision in the cornea, breaks up and removes the clouded lens and inserts a new artificial lens.
Glaucoma is then treated in the same operation. Various surgical methods are available, including
- Trabeculotomy: The surgeon cuts small holes in the trabecular meshwork or uses a laser to improve the drainage of the aqueous humour.
- Trabeculectomy: A small channel is created between the eye chamber and the conjunctiva of the eye to allow the aqueous humour to drain.
- Trabecular aspiration: The chamber angle is cleaned by irrigation with the trabecular meshwork.
Alternatives to combined glaucoma and cataract surgery
Although combined glaucoma and cataract surgery is often beneficial, it is not the only treatment option. Cataracts can also be treated independently of glaucoma by replacing the lens.
This operation often leads to a reduction in intraocular pressure. The lens of the eye thickens slightly with age, which can lead to a slight increase in intraocular pressure.
By replacing the old lens with a thinner artificial lens, this increase is corrected and the intraocular pressure can fall back to normal levels. If the intraocular pressure is slightly elevated, this may be sufficient and no further treatment is required.
It is also possible to carry out all treatments for glaucoma independently of cataract surgery. In this case, all the usual treatment options are available, including eye drops, surgery and various laser treatments as described above.
The temporal separation of cataract and glaucoma surgery offers several advantages. Firstly, the mild blood pressure lowering effect of cataract surgery can be awaited before specific measures are taken to treat the glaucoma.
In some cases, this may be enough to temporarily prevent the need for glaucoma surgery. In the past, the relatively traumatic nature of anti-glaucomatous surgery, which often resulted in fistula formation, also militated against combined procedures.
A supplement or alternative to glaucoma surgery: The Integrated Eye Therapy according to Noll
Innovative approaches to glaucoma treatment such as Integrated Eye Therapy according to Noll are of great importance in ophthalmology. Noll Eye Acupuncture has specialised in the treatment of chronic and degenerative eye diseases and, with its established procedure, offers a promising addition – or alternative – to conventional surgical methods.
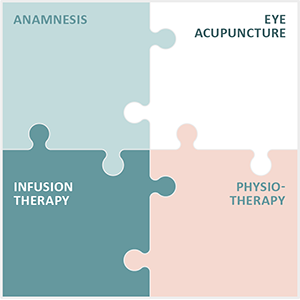
The therapy consists of the following four core elements:
- Comprehensive anamnesis: a detailed survey of the patient’s medical history in order to create an individualised treatment plan.
- Eye acupuncture according to Prof. John Boel: This special form of acupuncture is at the centre of the therapy and is intended to activate the eye’s self-healing powers.
- Customized infusions: Customized infusion therapies to support general eye health.
- Specialized physiotherapy: Measures to promote blood circulation and functionality of the eye.
These elements help to meet the needs of patients with chronic eye conditions and provide valuable support to conventional glaucoma treatment.
The practice is particularly proud of the positive feedback from patients who have experienced a significant improvement in their quality of life.