Pseudoexfoliation syndrome treatment (PEX glaucoma)
Pseudoexfoliation syndrome (PEX glaucoma) treatment – we give a complete overview of the different treatment methods for pseudoexfoliation syndrome
Pseudoexfoliation syndrome (PEX glaucoma)
Pseudoexfoliation glaucoma, also known as pseudoexfoliative glaucoma, is a common complication of pseudoexfoliation syndrome. PEX glaucoma is a type of secondary open-angle glaucoma with elevated intraocular pressure and has a higher rate of progression compared to other forms of glaucoma, meaning that it carries a greater likelihood of optic nerve damage.
There are some differences between PEX glaucoma and primary open-angle glaucoma. PEX glaucoma is characterised by more pigmentation in the chamber angle and higher intraocular pressure values. It tends to cause pressure peaks and fluctuations throughout the day as well as acute increases in pressure in conjunction with dilation of the pupil.
In addition, optic nerve damage and visual field loss occur more quickly and more frequently in PEX glaucoma. These differences in symptoms are also associated with greater resistance to drug therapy.
Around half of people with pseudoexfoliation syndrome also develop pseudoexfoliation glaucoma over time, making PEX syndrome one of the most common causes of glaucoma overall. Around a third of patients diagnosed with this form of glaucoma suffer from the condition in both eyes.
The deposits that occur with pseudoexfoliation syndrome in the lens of the eye and in the angle of the chamber lead to occlusion of the angle of the chamber. This in turn prevents the normal outflow of aqueous humour and leads to an increase in intraocular pressure. This increased pressure on the optic nerve increases the risk of damage, which ultimately leads to the development of glaucoma.
In advanced stages, pseudoexfoliative glaucoma, like all glaucomas, causes visual field loss. Compared to primary open-angle glaucoma, PEX glaucoma progresses more quickly and responds less well to drug treatment. Surgical intervention is therefore necessary in many cases.
Causes of pseudoexfoliation syndrome
The exact causes for the occurrence of pseudoexfoliation syndrome remain unclear in research. However, there are scientific studies that suggest various hypotheses:
One possible cause could lie in certain inflammatory reactions and processes that could favour the development of pseudoexfoliation syndrome. On the other hand, studies suggest that genetic factors and oxidative stress could play a significant role.
There are also indications that an increased homocysteine level could favour the occurrence of pseudoexfoliation syndrome. Homocysteine is an amino acid that is of interest in connection with cardiovascular diseases, especially cardiovascular diseases.
Furthermore, studies show that pseudoexfoliation syndrome occurs more frequently in patients with mutations in the LOXL1 gene. This gene plays a crucial role in elastin metabolism, and mutations can apparently lead to the production of pseudoexfoliative material.
However, it is important to emphasise that the presence of this gene defect is not the only factor contributing to the development of pseudoexfoliation syndrome, and it does not necessarily lead to the development of glaucoma.
Another significant factor in the development of pseudoexfoliation syndrome is age. The risk of developing this disease increases with age, especially in people over 70. In Switzerland, around one in 20 people are affected, with women being at a higher risk.
In view of the ageing population, the syndrome is becoming increasingly clinically significant in both women and men.
Diagnosis of pseudoexfoliation syndrome (PEX): Recognition and criteria
In the case of advanced pseudoexfoliation syndrome, the ophthalmologist can identify specific abnormal findings. With the aid of the slit lamp, for example, protein-like accumulations on the pupil margin and deposits on the lens of the eye can be identified.
In addition, an examination of the chamber angle, known as gonioscopy, can detect deposits of PEX material in the dense tissue of the chamber angle. These deposits can obstruct the natural outflow of aqueous humour.
The PEX material, which is formed in various parts of the eye both inside and outside, consists of fine-fibre, elastic components originating from various cells and tissues. In the eye, whitish, flaky particles are visible on the lens and its inner edge as well as on the iris.
The diagnosis of pseudoexfoliation syndrome can be challenging in many cases due to the absence of central deposits. A reliable diagnosis is often only possible after pupil dilation.
In the early stages, the presence of the disease can be recognised by factors such as subtle changes in the lens in combination with pigment dispersion (detachment of pigment cells from the back of the iris) or mydriasis weakness (pupil dilation dysfunction).
Due to the high risk of developing glaucoma, early diagnosis of PEX syndrome is highly desirable. Accurate and early diagnosis is particularly clinically relevant, especially when considering the potential need for cataract surgery (lens replacement surgery) as part of cataract treatment and the associated risks.
Clinical criteria for the diagnosis of pseudoexfoliation syndrome
The clinical criteria for the diagnosis of pseudoexfoliation syndrome include
- Disc-shaped deposits: of grey, flaky material on the front of the lens and in the angle of the chamber
- Iris flutter: which is characterised by tremor of the iris due to poor adhesion to the environment, for example, during head movements.
- Lens luxation: where the lens is displaced into the anterior chamber of the eye or into the vitreous cavity.
- Rubeosis iridis: a pinkish-red colouration of the iris or increased vascularisation in the iris and the angle of the chamber.
- Secondary optic atrophy: refers to the atrophy of nerve cells in the optic nerve.
Symptoms of pseudoexfoliation syndrome
Pseudoexfoliation syndrome often remains without recognisable symptoms and does not cause any pain. However, if complications such as glaucoma occur, symptoms can develop that can lead to damage to the optic nerve head and progressive vision loss.
But what risk factors increase the likelihood of developing pseudoexfoliation syndrome?
The risk of this disease increases significantly with age, especially in people over 70. In the population as a whole, on average around one in 20 people are affected, with women having a higher risk of developing the disease. With the steady increase in the average age of the population, the prevalence of pseudoexfoliation syndrome also increases.
Genetic predispositions also play an important role. People who have a family history of this disease are at increased risk. Living in northern countries can also increase the risk of pseudoexfoliation syndrome.
Overall, it is crucial to keep an eye on these risk factors and have regular ophthalmological examinations in order to recognise possible symptoms and signs at an early stage and take appropriate measures for prevention and treatment.
Treatment options for pseudoexfoliation syndrome
As the exact causes of pseudoexfoliation syndrome cannot be treated or are not yet fully understood, treatment is focussed on preventing further damage to the eye.
For example, if the intraocular pressure is elevated, attempts can be made to lower it with eye drops to reduce the risk of developing glaucoma. There are various types of eye drops available that are suitable for reducing intraocular pressure.
As a rule, treatment begins with an eye drop preparation containing only one active ingredient. If the reduction in intraocular pressure is not sufficient, a combination of several active ingredients can be considered. As a rule, however, no more than two different eye drop preparations with a total of three different active ingredients are used.
If there is an occluded chamber angle, an attempt can be made to open it using a laser to improve the outflow of aqueous humour in the trabecular meshwork. This procedure, known as selective laser trabeculoplasty, treats the trabecular meshwork with a laser beam, which enlarges the pores in the tissue and improves drainage.
Selective laser trabeculoplasty is a gentle procedure and can be used at the beginning of glaucoma therapy or in addition to the use of eye drops. If the effect of the laser procedure diminishes, the treatment can be repeated without any problems.
Normally, laser treatment can reduce intraocular pressure by around 30 per cent. However, this effect often does not last very long and the need for surgical intervention occurs more quickly than with other forms of glaucoma.
If the intraocular pressure cannot be reduced sufficiently, the only remaining option is to surgically remove the lens, which is known as cataract surgery. The removal of the lens offers the possibility of eliminating the cause of the pseudoexfoliation syndrome, which can lead to a normalisation of the intraocular pressure after the operation. Surgery should be considered particularly in cases of severe pressure fluctuations and the simultaneous presence of a cataract.
Standard procedures for surgical therapy
Here is an overview of the standard procedures for the surgical treatment of pseudoexfoliation syndrome:
Trabeculectomy (filter cushion surgery)
A small hole is made in the wall of the eyeball, which is covered with part of the sclera. This allows the aqueous humour to drain under the conjunctiva in the event of increased intraocular pressure, where a kind of drainage cushion is formed.
Canaloplasty (suture surgery)
This technique widens Schlemm’s canal using a microcatheter and a special gel and stretches a fine thread into the canal. This improves the drainage of the eye without opening the eyeball itself. However, canaloplasty does not usually achieve the same level of pressure reduction as trabeculectomy, which is why additional eye drops are often required.
iStent implant
In this minimally invasive procedure, two titanium implants are inserted into the chamber angle in the trabecular meshwork. This allows the aqueous humour to flow directly into Schlemm’s canal. The implantation can be performed alone or at the same time as cataract surgery to further reduce intraocular pressure.
XEN gel implant
This is a minimally invasive procedure in which a gelatin tube is inserted into the anterior chamber to create an ocular cushion, similar to trabeculectomy.
Drainage implants
If medication and trabeculectomy do not sufficiently reduce intraocular pressure, a silicone tube can be inserted into the anterior chamber to allow fluid drainage.
Cyclophotocoagulation
In this procedure, the ciliary body, which is responsible for the production of ocular fluid, is cauterised using a laser. This reduces the amount of fluid produced and lowers the intraocular pressure.
It should be noted that there are risks after both laser treatments and surgical procedures in the early post-operative phase. This is because inflammatory reactions and pressure peaks can occur when the blood-aqueous barrier breaks down.
These reactions occur frequently, so intensive monitoring and treatment during and after surgery is of great importance.
It is also important to note that the treatment of pseudoexfoliation syndrome is essentially the same as that of primary open-angle glaucoma. However, it is crucial to change the therapeutic approach more quickly and consistently from conservative to surgical measures.
Prognosis of pseudoexfoliation syndrome
The prognosis of pseudoexfoliation syndrome and the often associated glaucoma depends crucially on timely detection. Thanks to a wide range of individually adaptable treatment options, there is now a chance of a favourable prognosis. However, if left untreated, the syndrome can lead to premature blindness.
A comparison of the symptoms of patients diagnosed with pseudoexfoliation glaucoma with those of patients with primary chronic open-angle glaucoma at the time of detection shows that the average intraocular pressure is significantly higher in pseudoexfoliation glaucoma patients.
In addition, around a quarter of pseudoexfoliation glaucoma patients are practically blind in the affected eyes, while only around 15 per cent of those suffering from primary open-angle glaucoma show a slight deterioration in vision.
Furthermore, those affected by pseudoexfoliation syndrome are significantly more likely to have deposits in the chamber angle. Regular ophthalmological check-ups are therefore crucial for patients with pseudoexfoliation syndrome.
Pseudoexfoliation syndrome prevention
Pseudoexfoliation syndrome, although initially asymptomatic, can cause serious eye and vision damage, especially if increased intraocular pressure leads to glaucoma. This can lead to irreversible damage to the optic nerve and severe visual impairment. Early diagnosis is the key to preventing further damage.
To slow the progression of the disease, regular monitoring of intraocular pressure is crucial in patients with PEX syndrome, especially in the onset of glaucoma. If glaucoma is already present, consistent lowering of intraocular pressure is required and must be monitored in the daily pressure profile. The aim is to keep the pressure below 15.
Experience shows that patients with pseudoexfoliation syndrome and elevated intraocular pressure develop glaucoma much more frequently than patients with elevated intraocular pressure but without pseudoexfoliation syndrome. Drug treatment is therefore advisable even if the optic nerve and visual field are still normal.
The PEX material forms not only in the eye, but also in the skin, blood vessels and various organs. Possible links between PEX syndrome and various vascular diseases should therefore be considered.
Vascular risk factors for PEX syndrome may include transient ischaemic attacks, angina pectoris, hypertension, myocardial infarction and apoplexy. A connection with aneurysms is also suspected. If PEX syndrome is present, it is therefore recommended that a Doppler sonography, an ultrasound examination to measure the blood speed in the vessels, is carried out regularly.
Innovative approaches to the treatment of pseudoexfoliation syndrome at Noll Eye Acupuncture
Pseudoexfoliation syndrome (PEX) and the resulting PEX glaucoma are among the most serious chronic eye diseases that require specialised and differentiated treatment.
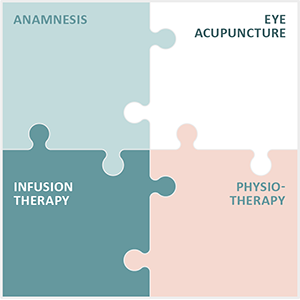
With the Integrated Eye Therapy according to Noll, Eye Acupuncture Noll offers a specialised treatment option that is tailored to the individual needs of patients and is based on a holistic view of the organism. Our approach combines:
- A careful anamnesis as the basis for a customised treatment concept
- Eye acupuncture according to Prof. Boel, which is at the centre of our therapy and is based on a long tradition and experience.
- Customised infusion therapies that are tailored to the individual deficits and needs of patients
- Specific physiotherapy that supports the body as a whole and is geared towards ophthalmological challenges.
These elements are incorporated into our treatment strategies for pseudoexfoliation syndrome and PEX glaucoma, recognising that each condition and each patient is unique.
Over the past 13 years, our practice has made a name for itself by supporting and guiding patients from all over the world. We emphasise responsible and respectful treatment without raising unrealistic hopes.
We are proud of the many positive testimonials on eye acupuncture we have received from patients and will continue to advocate for the well-being and vision of our patients.